- Posted by : exsure.in
- Uncategorized
As ubiquitous messengers, exosomes play a role in how our bodies manage energy. From adipocytes to the gut microbiome, new insights into how exosomes modulate human metabolism might be providing a glimpse into the future of metabolic disease treatment.
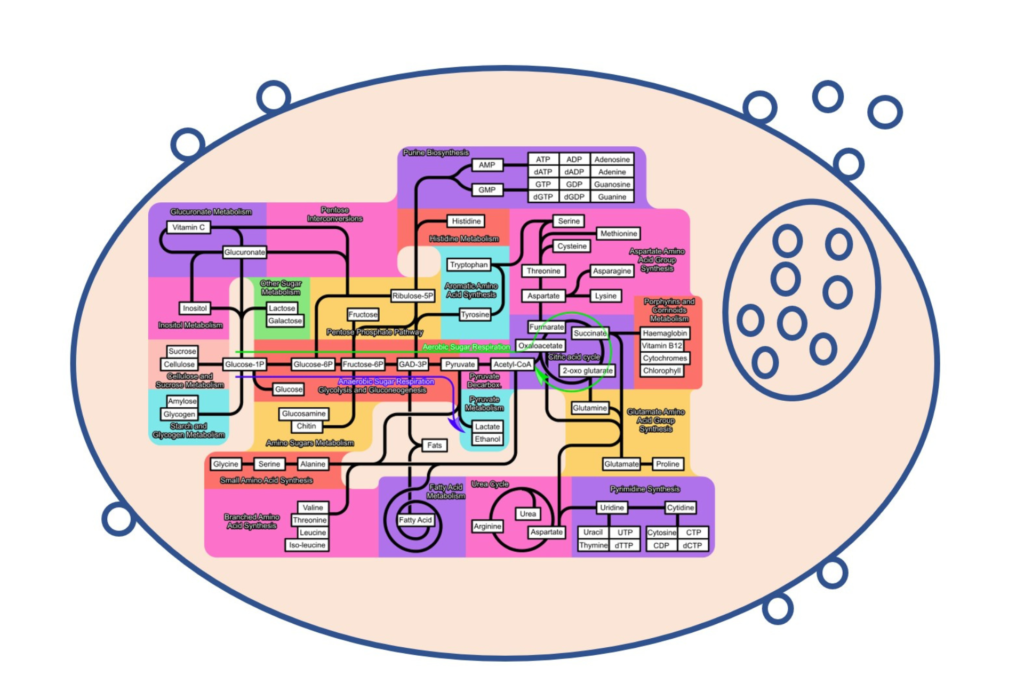
Metabolism is the body’s powerhouse, a highly complex process regulated by a multitude of endogenous and exogenous factors to generate the energy and building blocks necessary for cellular function. Communication among various metabolic organs and factors is vital for maintaining metabolic homeostasis and, in the face of rising rates of metabolic diseases, recent discoveries have shed new light on the role of exosomes as the new mode of cellular communication in this interplay.
Pancreatic β-cells are essential for regulating glucose homeostasis by secreting insulin in response to glucose, amino acids and fatty acids in the bloodstream. Exosomes released from islet cells and insulin-sensitive tissues contain various biomolecules, including proteins, lncRNAs and miRNAs, These play crucial roles in the regulation of glucose homeostasis and insulin resistance in other metabolic organs, as well as immune and endothelial cells. Interestingly, the exosomal miRNA cargo is not a mere reflection of the parental β-cell’s content, as a subset of miRNAs is preferentially released in exosomes, while others are retained in the parental cells.
Exosomes released by skeletal muscles may also play a role in the inter-organ network governing glucose homeostasis. Intravenous or intramuscular injection of muscle-derived exosomes into mice led to their accumulation in various metabolic tissues, including the pancreas, liver, gastrointestinal tract and distal muscles, indicating cross-talk between insulin-sensitive and insulin-releasing cells. Additionally, muscle-specific miR-206-containing exosomes released from skeletal muscles can promote β-cell proliferation in a mouse model of obesity to compensate for insulin resistance.
Endurance exercise has been found to cause an increase in circulating exosomes released by skeletal muscles and other tissues, suggesting their potential role in the autocrine and paracrine signals that lead to the systemic benefits of exercise. However, the precise mechanisms through which exosomes contribute to these benefits remain unclear.
Liver cells release exosomes that impact various liver functions. Hirsova et al. (2016) found that the liver cells release exosomes containing TRAIL in response to palmitate, which promotes macrophage activation and the release of pro-inflammatory cytokines via a RIP1 and NFκB-dependent mechanism. Additionally, an increase in liver exosome release was observed in the serum of mice fed a diet high in saturated fat, fructose and cholesterol. Blocking this exosome release reduced macrophage activation and hepatocyte inflammation.
Exosomes released by adipose tissue may also contribute to regulating blood glucose homeostasis. For instance, exosomes released by adipose tissue in obese mice have higher levels of RBP4 protein, leading to insulin resistance by activating the TLR4/NFκB pathway. Additionally, they lower Akt phosphorylation in response to insulin, reducing glucose transport. These observations were also found in human models, where a correlation was identified between the number of exosomes released by adipose tissue and the Homeostasis Model Assessment (HOMA) insulin resistance index.
Thomou et al. (2017) studied the regulatory role of miRNAs released in exosomes from different types of fat on gene expression in distant metabolic organs and demonstrated that the level of circulating exosomal miRNAs could be modified by transplanting various fat depots. For instance, transplanting brown adipose tissue (but not white adipose tissue) improved glucose tolerance and insulin sensitivity in mice by transferring miR-99b via exosomes to inhibit FGF21 expression in the liver.
Exosomes are also involved in regulating lipid transporters, such as ABCA1 and ABCG1, which are crucial for reverse cholesterol transport. Deficient cholesterol efflux due to the knockout of these transporters promotes foam cell formation in macrophages. Some circulating miRNAs found in exosomes, such as miR-30e and miR-92a, can inhibit these transporters, leading to intracellular cholesterol accumulation. Platelet-derived exosomes can inhibit cholesterol absorption by reducing CD36-dependent lipid loading of macrophages and suppressing platelet thrombosis.
Exosomes have been found to modulate the gut microbiome and impact host metabolism, as reviewed by Feng et al., (2021) and Zhang et al., (2022). Intestinal cell-secreted exosomes can contain antimicrobial peptides that selectively control microbiome composition. Additionally, exosomes can transfer genetic material between cells to alter gut microbiome gene expression and function. Exosomes also influence the host’s immune system by transferring immune-related molecules impacting the gut microbiome’s composition and activity. Additionally, gut microbiome-secreted exosomes interact with host intestinal cells, affecting cell signalling and gene expression while potentially contributing to the integrity of the intestinal mucus layer.
Overall, exosomes offer the potential for monitoring cellular metabolic states and delivering therapeutic agents, presenting a promising approach to treating metabolic diseases. However, their complex mechanisms, diverse biomolecules, and multiple effects on target cells pose challenges to developing safe and effective exosome-based therapies. More research is needed to understand these mechanisms and create effective treatments. Despite these challenges, the growing evidence of exosomes’ role in metabolic organ cross-talk opens new perspectives in inter-organ communication and therapeutic development.